Introduction
Blood transfusion is an integral part of routine outpatient Haematology-Oncology care. Blood product administration requires the concerted effort of nursing and laboratory staff in accredited institutions. One of the challenges with scheduling transfusions is the unpredictability surrounding transfusion requirements and the amount of time required to administer blood products. This mismatch between capacity availability for ad hoc transfusions and clinical need has resulted in physicians pre-booking transfusion slots so patients can be transfused if needed. However, when patients do not require transfusions, their cancelled slots represent capacity which could have otherwise been used to administer chemotherapy. This problem is exacerbated in a pandemic, where demand for inpatient beds necessitates the transition of elective chemotherapy to the outpatient setting insofar as is possible.
Aim
We hypothesized that reducing the number of transfusion slots booked could help to save healthcare-related costs and improve capacity utilisation. We also sought to right-site blood transfusions away from the chemotherapy infusion unit and to an acute cancer care unit (ACCU).
Methods
On 1 May 2020, two simple workflow changes were made. First, we introduced a policy where transfusions could not be pre-booked. Physicians were reassured that their patients would be transfused before their patient's crossmatch sample expired and that urgent transfusions would be done on the same day. The only exceptions to this policy were regularly transfused patients (e.g. thalassaemia major patients on chronic transfusions) and infirm patients. Secondly, ad hoc blood transfusions were moved from the chemotherapy unit to the acute cancer care unit. Ad hoc transfusion timing was prioritised according to clinical need.
Consecutive patients treated at the National University Cancer Institute, Singapore, from 1 July 2019 to 31 July 2020 were included. Scheduled appointments were extracted from the hospital's scheduling system and analysed. Patients who had appointments booked for blood product transfusions were included. Data was extracted from drug ordering systems to determine the number of blood products administered. Patients were divided into a historical control group (before 1 May) and a study group (after 1 May).
The primary outcome measures were cancellation rate (defined as the number of cancellations over total number of slots booked for transfusion) and number of chair hours wasted. Secondary outcome measures included the number of patients who had to be admitted for blood transfusion due to lack of slot availability and cost savings reflected in unit chair hours made available.
Categorical data were analysed by the chi-square test. Analysis was done with SPSS v22 (IBM, USA).
Results
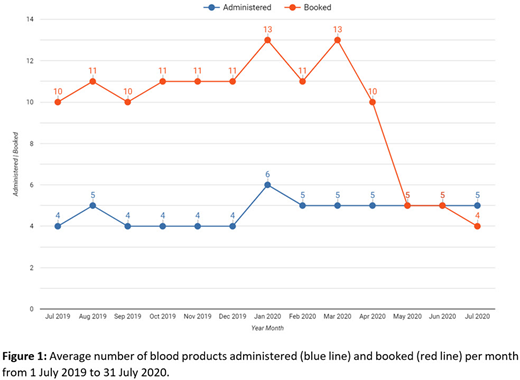
Between 1 July 2019 and 31 July 2020, a total of 3144 slots were booked for transfusion. Each slot was booked for four hours. 1548 blood products were administered.
In the control group, there were 1630 cancellations. This equated to 6520 hours of chemotherapy chair time (average of 652 hours/month). There were no nett cancellations in the study group, as total number transfused exceeded the number booked. Assuming the booking rate would have been similar without our intervention, the study resulted in 1956 unutilised chair hours saved. This reflects capacity created for administration of chemotherapy, and cost savings of 1956x, where x is the unit cost of one chair hour.
The cancellation rate was 58.3% (1630 cancelled, 2800 booked) in the control group. This decreased to -9.9% in the study group (378 administered (i.e., no nett cancellations), 344 booked, p<0.001, Figure 1). No patients had to be admitted for elective blood transfusion after 1 May 2020. One patient had to be admitted emergently for blood transfusion because of concurrent cardiac failure. The primary reason for admission was intravenous diuresis. All ad hoc transfusions were administered in ACCU.
Conclusion
Efficient utilisation brought about by two simple workflow changes can help to create capacity and save costs. Such strategies are especially critical in a pandemic, where healthcare resources are under major strain and existing capacity must be maximised.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal